Back Pain Treatment Guide in the U.S.: Causes, Therapies, and Recovery Approaches
Back pain remains one of the most common health issues in the United States, affecting millions of adults and limiting daily activities. By late 2025, U.S. healthcare discussions emphasize both traditional and modern approaches to treating back pain, reflecting a growing interest in sustainable relief. This guide examines the condition comprehensively—from understanding underlying causes and reviewing treatment methods to highlighting recovery strategies and associated considerations—helping individuals stay informed about long-term spinal health.
What Are the Common Causes of Back Pain in Adults?
Adult back pain typically stems from several distinct sources, each requiring different treatment approaches. Muscle strains and ligament sprains represent the most frequent causes, often resulting from improper lifting, sudden movements, or poor posture. These soft tissue injuries usually affect the lower back and can cause significant discomfort for days or weeks.
Degenerative disc disease occurs when spinal discs lose their cushioning properties over time, leading to pain and stiffness. Herniated discs, where the inner gel-like material pushes through the outer disc wall, can compress nearby nerves and cause radiating pain. Spinal stenosis, a narrowing of the spinal canal, commonly affects older adults and can result in back pain accompanied by leg symptoms.
Other contributing factors include arthritis, osteoporosis, scoliosis, and lifestyle elements such as obesity, sedentary behavior, and occupational hazards. Stress and psychological factors can also influence pain perception and recovery times, highlighting the complex nature of back pain conditions.
What Non-Surgical and Surgical Treatment Methods Are Available?
Non-surgical treatments form the foundation of back pain management and prove effective for most patients. Physical therapy remains a cornerstone approach, combining targeted exercises, manual therapy, and education to improve strength, flexibility, and movement patterns. Healthcare providers often recommend anti-inflammatory medications, muscle relaxants, or prescription pain medications for acute episodes.
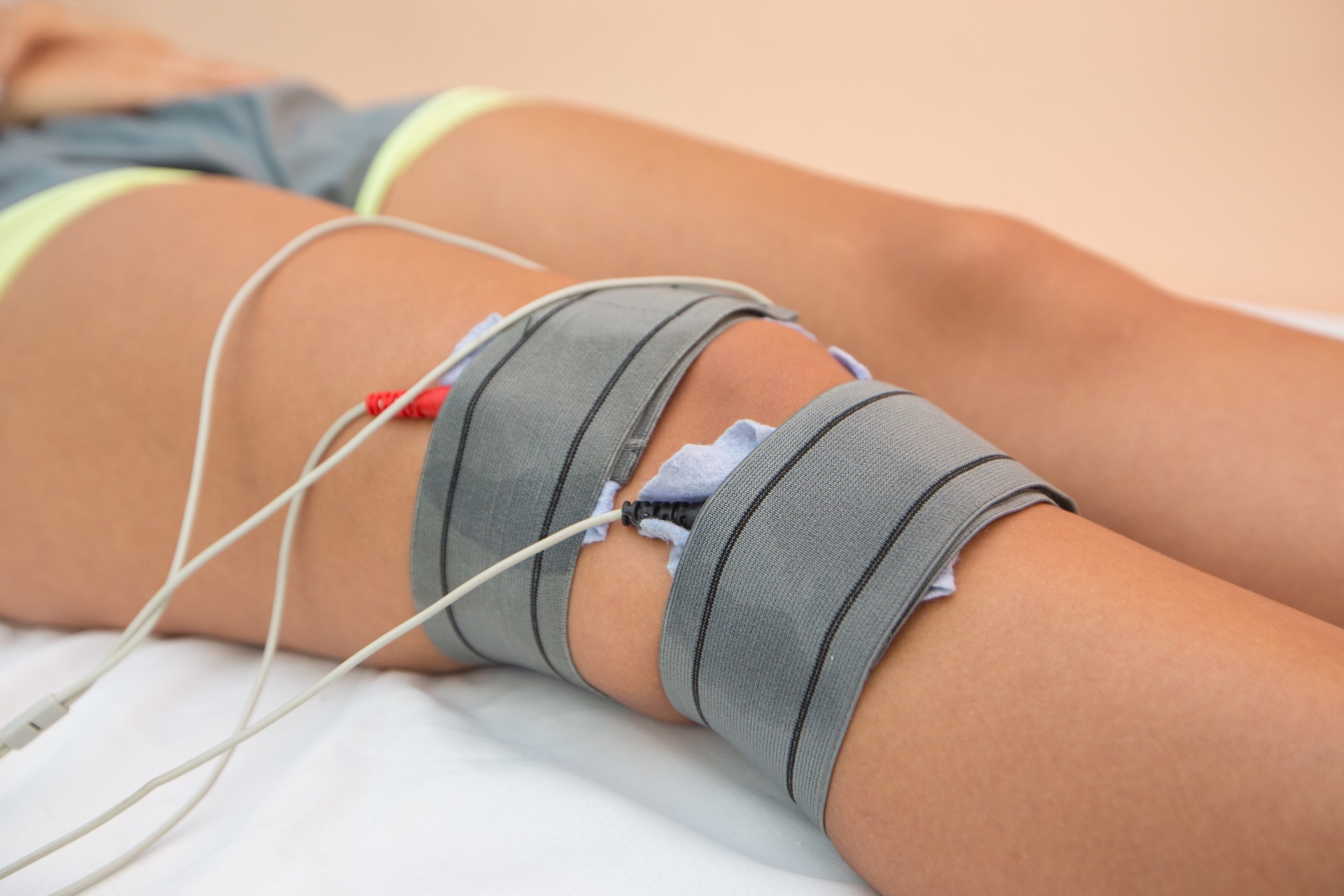
Heat and cold therapy, massage, acupuncture, and chiropractic care offer additional non-invasive options. Epidural steroid injections can provide temporary relief for specific conditions involving nerve inflammation. Lifestyle modifications, including weight management, ergonomic improvements, and stress reduction techniques, support long-term pain management goals.
Surgical interventions become considerations when conservative treatments fail to provide adequate relief after several months, or when serious neurological symptoms develop. Common procedures include discectomy for herniated discs, laminectomy for spinal stenosis, and fusion surgery for instability issues. Minimally invasive techniques have reduced recovery times and complications compared to traditional open surgeries.
How Do Recovery Strategies and Physical Therapy Pathways Work?
Recovery from back pain involves a structured approach that typically begins with acute pain management and gradually transitions to restoration of function and prevention of recurrence. The initial phase focuses on controlling pain and inflammation while maintaining basic mobility. Healthcare providers often recommend modified activities rather than complete bed rest, as prolonged inactivity can delay healing.
Physical therapy pathways are customized based on individual conditions, fitness levels, and treatment goals. Early-stage therapy emphasizes gentle movements, posture education, and basic strengthening exercises. As recovery progresses, therapists introduce more challenging exercises targeting core stability, flexibility, and functional movements that mirror daily activities.
Advanced recovery strategies incorporate work hardening programs for individuals returning to physically demanding jobs, sport-specific training for athletes, and ongoing maintenance programs to prevent future episodes. Patient education plays a crucial role throughout the recovery process, teaching proper body mechanics, exercise techniques, and self-management strategies.
Healthcare providers often coordinate multidisciplinary teams including physicians, physical therapists, occupational therapists, and pain management specialists to optimize recovery outcomes. Regular monitoring and treatment plan adjustments ensure that recovery strategies remain aligned with patient progress and changing needs.
The recovery timeline varies significantly depending on the underlying condition, treatment approach, and individual factors. Acute muscle strains may resolve within weeks, while more complex conditions requiring surgery can involve months of rehabilitation. Setting realistic expectations and maintaining consistent engagement with prescribed treatments significantly influence recovery success rates.
Modern recovery approaches emphasize active participation rather than passive treatments, encouraging patients to take ownership of their healing process. This philosophy has shown improved outcomes in both short-term pain relief and long-term functional restoration, making it a preferred approach among healthcare providers treating back pain conditions.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




